INTRODUCTION
- Wasting is prevalent among patients with chronic kidney disease
(CKD)
- About 18% to 75% of adults with end-stage renal disease
(ESRD) undergoing maintenance dialysis showed some evidence of wasting
- Although inadequate nutrition may contribute to wasting or
cachexia, other factors including systemic
inflammation, perturbations of appetite-controlling hormones from reduced renal
clearance, aberrant neuropeptide signaling, insulin and insulin-like growth factor
resistance, and metabolic acidosis, may be important in the pathogenesis of
CKD-associated wasting
- The wasting/cachexia
syndrome in CKD patients consists of anorexia, increased energy
expenditure, decreased protein stores characterized by a low serum albumin, and
loss of body weight and loss of muscle mass
- Importantly, the individual components of this syndrome
all represent risk factors for mortality
in patients with CKD, which is 100–200 times higher than the general population
- The wasting/cachexia syndrome should be distinguished from
malnutrition:
DIAGNOSTIC CRITERIA OF CACHEXIA/PROTEIN-ENERGY WASTING IN CKD
- Cachexia was defined as “a complex metabolic syndrome
associated with underlying illness and characterized by loss of muscle, with or
without loss of fat” (Evans et al., 2008)
- In the context of CKD, the term protein–energy wasting (PEW) has been proposed by The International
Society of Renal Nutrition and Metabolism (ISRNM) to describe a “state of
decreased body stores of protein and energy fuels (body protein and fat masses)”
- The ISRNM suggested that the term cachexia be reserved for
only the most severe forms of PEW. However, there is no obvious distinction between PEW
and cachexia from a pathophysiology standpoint
- Limiting the term cachexia to the extreme forms of PEW could
be considered too restrictive. The term pre-cachexia has been proposed to
include the milder forms of wasting in cancer patients (Fearon et al., 2011)
- Cachexia Definition
(Evans et al., 2008)
- Protein-energy wasting in CKD (by ISRNM, Fouque et al.,
2008)
DIAGNOSTIC CRITERIA
OF CACHEXIA/PROTEIN-ENERGY WASTING IN CKD (cont’)
Anthropometric
Indicators
1) BMI
- Although BMI gives little information about body
composition, BMI is a useful means of assessing PEW.
- BMI is strongly correlated with LBM at the low end of the
BMI spectrum, and low BMI is a consistent predictor of mortality in both adults
and children on maintenance dialysis.
- However, BMI is not a very precise parameter of
nutritional status in patients in whom gross imbalances in fluid homeostasis
are commonly observed, such as in patients with ESRD, CHF, and liver disease.
- Furthermore, in patients with significant muscle wasting
with relatively well-preserved fat mass, small changes in BMI may well be obscured
by imbalances in fluid homeostasis
2) SGA
- Stenvinkel et al. analyzed 268 patients with ESRD
according to their BMI and SGA,
- They found that 38% of their patients in the low BMI group had a normal SGA, whereas 45% of the patients in the normal BMI group and 17% in the high BMI group were considered to have PEW by SGA
- Low BMI has no impact on cardiovascular mortality whereas
an SGA ≥2 was associated with a marked increase in
cardiovascular mortality
3) Rate of weight
loss
- Unintentional weight loss or reduction in weight of 5% or
more over 3 months, or 10% or more over 6 months are suggested as indicators of
cachexia/PEW, independent of absolute BMI
4) Growth Failure in
Children
- Linear growth failure in children with CKD was highlighted
as central to the diagnosis of cachexia, and has been associated with a greater
mortality risk in children on maintenance dialysis
- However, the etiology of growth retardation in CKD is
multifactorial, including other factors such as delayed sexual maturation, bone
disease, acidosis, and growth hormone/insulin growth factor resistance.
- Growth failure may emerge as a necessary, but insufficient
criterion, for PEW in children with CKD
5) Muscle mass
- Reduced muscle mass appears to be the most valid criterion
for the presence of PEW in CKD, and is also emphasized in the diagnostic
criteria for cachexia.
- Mid-arm circumference has been shown to correlate with quality
of life and survival in adult patients on maintenance hemodialysis (HD).
- Dual X-ray absorptiometry, near-infrared interactance, and
bioelectrical impedance have been used in investigations of ESRD patients [30]
but these techniques have limitations in
ESRD and are not currently accepted as clinically useful tools.
- Indirect measures, such as creatinine appearance (estimated
by quantification of creatinine in a 24-h urine collection and in the collected
spent dialysate) have been proposed as an index of muscle mass in patients with
CKD and ESRD
6) Fat mass
- Body fat mass lower than 10% of body weight is considered
an additional criterion for PEW in adults with CKD due to the known
association between total body fat below 10% and increased mortality risk in
adult maintenance dialysis patients
- A more recent study showed that higher fat mass in
dialysis patients might actually be protective in survival predictability
- Nevertheless, abdominal fat deposition was shown to be
linked to inflammation and PEW, resulting in an increased mortality risk in maintenance
HD patients
Biochemical
Indicators
1) Albumin
- Low serum albumin is a consistent predictor of mortality
in both adult and pediatirc ESRD patients.
- A low serum albumin concentration is by far the strongest
predictor of mortality and poor outcomes in adult ESRD patients on maintenance dialysis
when compared to any other risk factors, including traditional risk factors
(hypertension, smoking, hypercholesterolemia, diabetes, and obesity) and nonconventional
ones (anemia measures, oxidative stress, minerals and bone surrogates, dialysis
treatment and technique)
- Dialysis patients with baseline serum albumin of even 0.2
g/dL higher or lower than other dialysis patients with similar demographic and
comorbidity constellations have significantly lower or higher death risk,
respectively.
- The albumin–death association is highly incremental and
linear, and the mortality–predictability of serum albumin below 4.0 g/dL has
virtually no cutoff level, below which the association with death would cease
or reverse
2) Prealbumin
- Low serum prealbumin (e.g., <30 mg/dL) is another
indicator of PEW and a strong predictor of outcomes in maintenance dialysis
patients
- Even though baseline serum prealbumin may not be superior
to albumin in predicting mortality in maintenance HD patients, prealbumin
concentrations <20 mg/dL are associated with death risk even in
normoalbuminemic patients, and a fall in serum prealbumin over 6 months is
independently associated with increased death risk
- Dialysis patients with high serum prealbumin have lower
proportion of body fat as well as higher proportion of muscle mass, which
suggest that normal serum prealbumin is associated with reversal of the abnormal
body composition in cachexia
- Dialysis patients with a baseline serum prealbumin between
20 and 40 mg/dl, a drop of 10 mg/ dl was associated with 37% increase in death
risk independent of baseline markers of malnutrition inflammation score (MIS),
serum albumin, and inflammatory markers
Food & Nutrition
Indicator (Anorexia)
- Both subjectively reported anorexia as well as measured
low protein or energy intake has been associated with increased mortality in
adult ESRD patients
- Anorexia is prevalent, in 30–40% in adult maintenance HD
patients, and is associated with higher concentrations of pro-inflammatory
cytokines and higher levels of erythropoietin hypo-responsiveness as well as
poor clinical outcome, including a fourfold increase in mortality, greater hospitalization
rates, and poor quality of life.
- As male ESRD patients seem to be more prone to
inflammation-associated anorexia than female patients, sex hormones may play an
important role in this context.
-Anorexia is prevalent in children with fairly mild CKD can
be the primary reason for growth failure
- Poor growth due to inadequate intake has been observed in
children with glomerular filtration rate as high as 70 ml/min/1.73m2
- Growth of children with CKD is compromised when energy
intake fall below 80% of recommended daily allowance.
Other indicators
- Serum transferrin, choleteral, inflammatory markers such
as CRP, proinflammatory cytokine such as IL-6.
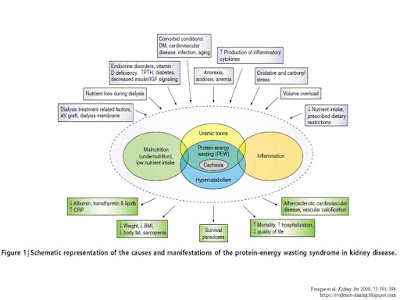
PATHOPHYSIOLOGY OF
CACHEXIA/PEW SYNDROME IN ADVANCED CKD
- The pathophysiology of cachexia/PEW syndrome is CKD is multifactorial.
An overview is summarized in Figure below. Please refer to the original paper for
detailed discussion on Anorexia, Increased energy expenditure, Inflammation,
Insulin resistance and Vitamin D deficiency
THERAPEUTIC
STRATEGIES FOR PREVENTION AND/OR TREATMENT OF CACHEXIA/PEW IN CKD
1) Nutritional supplementation
- There is evidence that nutritional therapy will improve PEW
in adult ESRD patients, such as the use of oral nutritional supplement (ONS), Intradialytic
parenteral nutrition (IDPN) --> improved serum albumin and/or prealbumin level.
- Growth of children
with CKD is compromised when energy intake fall below 80% of recommended daily
allowance (RDA). Increasing energy intake to 100% (but not more than 100%) of
the RDA can increase weight gain and stabilize growth rates
2) Exercise &
Physical Activity
- While that is evidence that patients with ESRD can improve
skeletal muscle quality by exercise, longer training durations or more
sensitive analysis techniques are required before this regimen can be
recommended as therapy for cachexia/PEW in CKD.
- There is no data on whether exercises capacity tests can
predict outcome in ESRD.
3) Appetite stimulant
- Megestrol acetate is a synthetic derivative of
progesterone. Megestrol acetate may induce appetite via stimulation of
hypothalamic neuropeptide Y, modulation of calcium channels in hypothalamic
appetite centers or inhibition of inflammatory cytokines such as IL-1, IL-6, and
TNF
- In the only double-blinded,
crossover study of 24 maintenance hemodialysis patients with anorexia, no significant
increase in albumin or LBM was observed. A large number of side-effects were
reported, including headaches, dizziness, confusion, diarrhea, hyperglycemia, thrombo-embolism,
uterine bleeding, peripheral edema, hypertension, and adrenal insufficiency
- Thus, the current experience in ESRD patients does not
support the use of megestrol acetate in clinical practice.
4) Correction of
Acidosis
- There is evidence that acidosis can induce muscle protein catabolism
and it could therefore be an important factor contributing to loss of muscle
protein in these conditions
- Acidosis is associated with negative nitrogen balance and
degradation of branched-chain amino acids and protein
- There are, however, few treatments available for
correcting metabolic acidosis apart from alkali supplements such as NaHCO3
which, in CKD patients, carry the risk of sodium loading and fluid overload
- Despite the risk, a recent study using NaHCO3 supplementation
in patients with (predialyss) CKD actually led to a slower decline in their
renal function as well as improvement in their nutritional status (dietary
protein and calorie intake increased, accompanied by improvements in serum
albumin and LBM as assessed by mid-arm muscle circumference)
5) Growth Hormone
- Acquired resistance to the anabolic actions of growth hormone
(GH) is a potential cause of the increased net protein catabolism and wasting
in patients with advanced CKD.
- Studies showed that pharmacologic doses of recombinant
human growth hormone (rhGH) improves whole body protein homeostasis in chronic
HD patients in the short-term.
- More studies are needed to evaluate its long-term effect
of rhGH on outcomes in patients with advanced CKD
6) Ghrelin agonists
- The salutary effects of ghrelin on food intake and meal appreciation
suggest that it could be an effective treatment for anorexic ESRD patients
- Tolerance in appetite-regulating centres and/or other
factors may override the long-term appetite-stimulating effects of ghrelin
- Ghrelin infusion acutely induces lipolysis and insulin
resistance independently of GH and cortisol, thus it will be important to
follow subjects for the risk of diabetes while on long-term ghrelin treatment
- A major limitation of treatment based on natural hormones
is the need for parenteral administration, because of the large size of the
molecule. The long-term therapeutic potential of GHS-R agonists will likely
rest with orally bioavailable compounds
- Despite reports of the short- and intermediate-term
success of ghrelin administration in treating anorexia and cachexia in ESRD
patients, we must await results of studies on its long-term efficacy
7) Leptin and
melanocortin signalling modulation
- Studies in mice shows promising results, human studies are
awaited.
8)
Ubiquitin-proteasome inhibitors
- Cachexia/PEW in CKD is characterized by protein
catabolism. Protein synthesis is unchanged while protein degradation is
increased in CKD. The daily rate of protein turnover in cells is so high that
even a small increase in protein degradation will cause marked protein
depletion over time.
- The mechanism of increased protein degradation in CKD is through
the activation of the UPS.
- Complications of CKD, including acidosis, insulin
resistance, inflammation, and increased glucocorticoid and angiotensin II
production, all activate the UPS to degrade muscle protein
- Recognition of the role of the UPS in the pathogenesis of
cachexia/wasting has led to the therapeutic use of bortezomib—a proteasome
inhibitor—in cancer patients.
- Inhibition of the proteasome will block activation of
NF-[kappa]B, which is a common final pathway for signal transduction of many cytokines,
thought to be a central mechanism of cachexia/wasting in many chronic disease
states including CKD
9) Dose &
frequency of dialysis
- A recent randomized controlled trial failed to confirm the
beneficial effects of daily HD on nutritional status in maintenance HD
patients, as measured by serum albumin
CONCLUSION
- Many questions remain about the description,
classification, and treatment of PEW or cachexia in children and adults with
CKD.
- Whether nutritional supplementation can improve
nutritional status and hence morbidity and mortality in ESRD patients remains
to be tested with appropriately designed RCTs
- Most of the information on the novel strategies is
currently at the experimental level and awaits confirmation by RCTs in patients
with CKD-associated cachexia/PEW syndrome.
Further Reading:



My life is beautiful thanks to you, Mein Helfer. Lord Jesus in my life as a candle light in the darkness. You showed me the meaning of faith with your words. I know that even when I cried all day thinking about how to recover, you were not sleeping, you were dear to me. I contacted the herbal center Dr Itua, who lived in West Africa. A friend of mine here in Hamburg is also from Africa. She told me about African herbs but I was nervous. I am very afraid when it comes to Africa because I heard many terrible things about them because of my Christianity. god for direction, take a bold step and get in touch with him in the email and then move to WhatsApp, he asked me if I can come for treatment or I want a delivery, I told him I wanted to know him I buy ticket in 2 ways to Africa To meet Dr. Itua, I went there and I was speechless from the people I saw there. Patent, sick people. Itua is a god sent to the world, I told my pastor about what I am doing, Pastor Bill Scheer. We have a real battle beautifully with Spirit and Flesh. Adoration that same night. He prayed for me and asked me to lead. I spent 2 weeks and 2 days in Africa at Dr Itua Herbal Home. After the treatment, he asked me to meet his nurse for the HIV test when I did it. It was negative, I asked my friend to take me to another nearby hospital when I arrived, it was negative. I was overwhite with the result, but happy inside of me. We went with Dr. Itua, I thank him but I explain that I do not have enough to show him my appreciation, that he understands my situation, but I promise that he will testify about his good work. Thank God for my dear friend, Emma, I know I could be reading this now, I want to thank you. And many thanks to Dr. Itua Herbal Center. He gave me his calendar that I put on my wall in my house. Dr. Itua can also cure the following diseases ... Cancer, HIV, Herpes, Hepatitis B, Inflammatory Liver, Diabetis, Bladder Cancer,Colorectal Cancer,HPV,Breast Cancer,Kidney Cancer,Prostate Cancer,Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Alzheimer's disease,
ReplyDeleteDementia.Weak Erection,Love Spell,Leukemia,Lun,Fribroid,Infertility,Parkinson's disease,Inflammatory bowel disease ,Fibromyalgia, recover your ex. You can contact him by email or whatsapp, @ .. drituaherbalcenter@gmail.com, phone number .. + 2348149277967 .. He is a good doctor, talk to him kindly. I'm sure he will also listen to you.